Pregnancy, COVID-19 and You
ATTENTION (15/09/2020): Flu vaccine season begins in September. If you are pregnant, contact your GP about booking an appointment to help keep you and your baby safe - especially since little is known on how influenza and coronavirus infections may interact with each other to possibly worsen illness.
Information for those who are pregnant
Although a time of great joy, pregnancy also comes with its moments of anxiety and worry. Add the COVID-19 situation into the mix and it can feel like a very scary time at present.
The situation continues to change very quickly and the many sources of news and information can be difficult to stay on top of. We all have many questions in our heads. To help you work out what you need to know, we have gathered what is currently known* about the virus and the guidance that has been given to pregnant women or those planning a pregnancy.
*We’ll keep the information on this page updated as the situation unfolds and more information becomes available.
This article was last updated on: 11th October, 2020.
What is COVID-19?
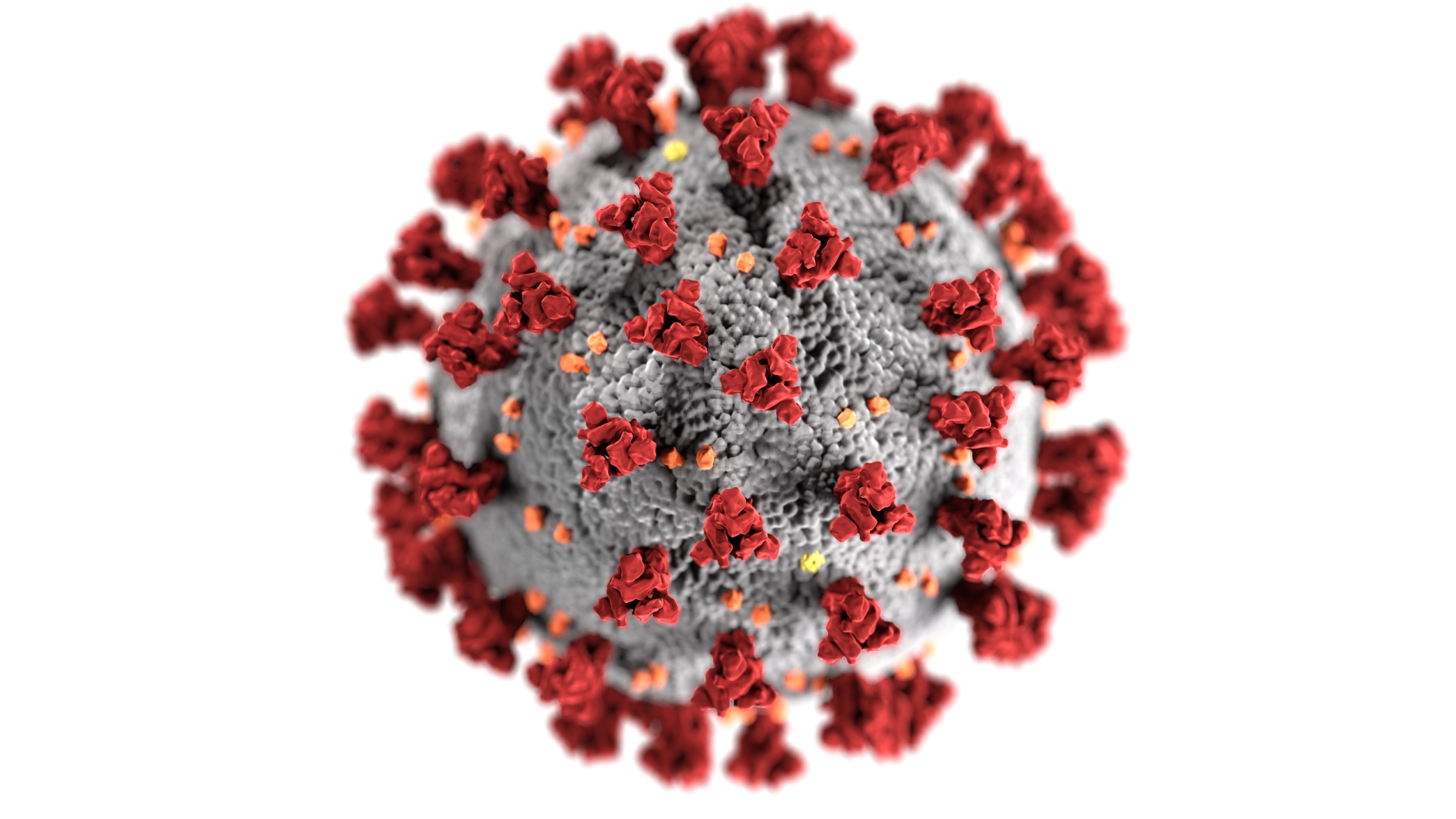
Image by CDC
Some of the current terminology can be confusing, but COVID-19 is the code-name given to this new disease. “COVID” is short for coronavirus disease and “19” indicates it was first detected in 2019.
COVID-19 is caused by a virus with the scientific name severe acute respiratory syndrome coronavirus 2 (or known by the shorter name, SARS-CoV-2).
Viruses are present in the environment and need a host body – animal or human – to survive. Outside the body, viruses are killed by soap, which is why it is important to wash your hands, disinfect surfaces and “catch” coughs and sneezes in your elbow or handkerchief to help stop the spread of the virus.
Once a virus enters the body, it is up to the immune system to kill it. Viruses like SARS-Cov-2 enter the host through the mouth, nose, eyes, or breaks in the skin, which is why it is important to keep your distance. Once inside the body, they attack the cells lining the respiratory system causing symptoms including: fever, a persistent dry cough, fatigue and difficulty in breathing.
Whilst most healthy people are able to fight off the infection with rest at home, there are high-risk groups such as the elderly and people with weakened immune systems who are more susceptible to severe infections and are unable to fight off the virus as easily.
What do I need to know if I’m pregnant?
In an effort to protect specific communities, pregnant women have been advised to stay at home during the COVID-19 outbreak as a precaution. However, England’s Chief Medical Officer, Professor Chris Whitty says “I certainly don’t think pregnant women should start worrying about this”. He went on to say that including pregnant women in the vulnerable group is “a precautionary measure because we are early in our understanding and we want to be sure."
This guidance, for pregnant women to stay at home, was first published on the 21st of March. It is based on what has been learnt from other respiratory infections, such as influenza and SARS, which is that pregnant woman who develop significant respiratory infections in the third trimester are more likely to become seriously unwell. This may also result in the need to deliver a women’s baby early, to enable the mother to recover.
Despite the guidance including pregnant women as a high-risk group, the overwhelming majority of current research (including the large INTERCOVID study from the University of Oxford) suggests pregnant women are at no greater risk from COVID-19 than non-pregnant women, and the majority of pregnant women who become ill with COVID-19 will have mild cases. However, a recent US study, PRIORITY, found that pregnant women may be more likely to experience prolonged symptoms of COVID-19.
Furthermore, the Royal College of Gynaecologists & Obstetricians report that there is currently “no evidence to suggest that COVID-19 causes problems with the baby’s development or causes miscarriage”. They add that no previous coronavirus strains (strains which are similar to the virus causing COVID-19) have been shown to cause abnormalities in the unborn baby.
What about evidence that COVID-19 can be passed from a mother to her unborn baby (referred to as “in utero” or “vertical” transmission)? Very recent research shows that transmission from mother to newborn cannot be ruled out. A case study published in The Pediatric Infectious Disease Journal suggests that a prematurely born girl in Texas may have contracted COVID-19 from her mother in the womb (more details in the Research Summary section at the bottom of this article). Another study by scientists in Wuhan, China examined 33 children born to mothers with COVID-19 and found three newborns had COVID-19 symptoms, but after seven days all three tested negative (i.e. clear) of the virus. Whether or not in utero transmission is possible with COVID-19, the risk appears to be very small, with the vast majority of newborns across similar studies testing negative for the virus after being birthed by infected mothers.
How will COVID-19 affect my birth plan?
Maternity Unit services, like other areas of the NHS, are experiencing COVID-19-related pressures to their workforce. As a result of this and as a precaution to keep you safe, some NHS Trusts and Boards suspended homebirth and waterbirth services at the peak of the pandemic, but most of these services have now been reinstated.
The NHS previously also introduced restrictions on birth partners, but these have since been eased, with some variation in the exact policies depending on which hospital and region you are in, as well as the COVID-19 "surge" level (a measure of how much of the hospital's capacity is occupied by COVID) at the time.
- England: policies may differ depending on the hospital, but NHS England advises that you should be able to have a birth partner provided they wear a mask, do not have COVID-19 symptoms and have not recently tested positive for the virus.
- Wales and Northern Ireland: government guidelines allow for one birthing partner, although hospitals may adjust their rules based on changing COVID-19 surge levels.
- Scotland: women may have two birthing partners if requested.
Pregnant women are advised to give birth at Maternity or Midwifery Units within hospitals, as availability of homebirth midwives cannot be guaranteed at this time. Pregnant women who – despite the official advice - still wish to have a homebirth are advised to seek advice from their doctor or midwife well before their delivery due date.
Pregnant women who have suspected or confirmed COVID-19 will be advised to have a hospital birth, to help ensure they and their baby will be safe.
COVID-19 illness is not currently changing the way you give birth, unless it has affected your breathing to the point where urgent caesarean delivery is required. The use of epidural and spinal blocks during labour are still appropriate options for most women.
However, if you have a suspected or confirmed case of COVID-19, the use of gas and air (Entonox) may increase the chance of the virus becoming airborne (in small droplets), something your medical team will want to avoid. You will be informed in early labour of your delivery options, with their benefits and potential risks, to help you make your decision.
Is it safe to breastfeed my baby?
For those who can, breastfeeding is an effective way to not only nourish your baby, but also to help develop their immune system. Our babies are not born with a fully functioning immune system, but the antibodies (microbe-fighting proteins) transferred from mother to child during breastfeeding can help to protect a baby until they are ready to protect themselves. Public Health England (PHE) advises that while this is a personal decision to discuss with your health advisor, mothers who test positive for COVID-19 should still breastfeed if possible.
Current research shows no evidence that the virus can be passed to the baby through breastmilk and the protective benefits of breastfeeding are thought to far outweigh the risk of transferring the virus through breastfeeding. PHE recommends the following precautions for infected mothers who choose to breastfeed:
- Washing your hands before touching the baby, breast pump or bottles
- Avoiding coughing or sneezing over the baby while you are breastfeeding
- Cleaning any breast pump, as recommended by the manufacturer, after each use
- Consider asking someone who is virus-free to bottle-feed your expressed breastmilk to your baby
- If you are feeding with formula or expressed milk, sterilise the equipment carefully before each use. You should not share bottles or a breast pump with anyone else.”
What do I need to know if I’m a pregnant healthcare worker?
Current guidance for pregnant healthcare workers is that they should make a choice whether to continue working in a patient-facing role. Your choice – whether to continue working in a patient-facing role or not - must be supported by your employers. Those workers who choose to continue working in a patient-facing capacity should take all necessary precautions to protect themselves from COVID-19 by following the most up-to-date guidelines. Pregnant healthcare workers with underlying health conditions, or who are in their third trimester, are strongly advised to avoid patient contact.
Dr Jenny Harries, Deputy Chief Medical Officer, has said:
“The Government has taken the precautionary approach to include all pregnant women in a vulnerable group. This guidance will give pregnant healthcare workers the ability to make an informed choice about how they can continue to make an active and valuable contribution to the huge challenge facing us, whether at home or in the workplace.”
What do I need to remember?
The COVID-19 pandemic may make pregnancy a worrying time, but remember that at this stage, the guidelines issued for pregnant women are a precaution to keep you and your baby safe. Help yourself by eating healthily, getting a good night’s sleep and keeping your stress levels low. Always make sure you talk to someone and reach out to your support network if you are feeling anxious or unhappy.
Please keep in mind that at the moment:
- Pregnant women do not seem to be more prone to contracting COVID-19
- Pregnant women do not seem to be more likely to severe forms of COVID-19
- COVID-19 does not seem to induce problems in pregnancies such as preterm (premature) labour or miscarriage
- COVID-19 is seemingly unlikely to be transmitted from the mother to her unborn baby
- COVID-19 does not seem to be transferred via breastmilk
For more information:
- The Royal College of Obstetricians and Gynaecologists website
- Public Health England website
The guidance is based on what experts know about the COVID-19 pandemic so far and from evidence gathered from other similar viral illnesses. More evidence is being collected and the guidance will be updated when this is available.
Please let us know if you think any content on this site is factually incorrect.
Below is a summary of the research currently available regarding COVID-19 in maternity
The University of California, San Francisco and the University of California, Los Angeles PRIORITY study, United States (SUMMARY, JOURNAL LINK)
A cohort study of 991 pregnant women in the US found that pregnant women with COVID-19 may present with prolonged symptoms that are slightly different to those experienced by non-pregnant COVID-19 patients.
Key findings:
- The majority of infected pregnant women have mild cases of COVID-19
- Pregnant women are less likely to experience fever as an early symptom
- Pregnant women are more likely to experience COVID-19 symptoms for a longer period of time than the average patient (two months or longer)
The University of Texas Southwestern Medical Center, United States (SUMMARY, JOURNAL LINK)
A case study of a preterm infant born to a COVID-19 positive mother suggests the infant contracted COVID-19 while still in the womb.
Samples of the baby’s placenta tested positive for the COVID-19 virus, as did the baby's nasal/throat swabs when tested 24 hours after birth.
University of Oxford INTERCOVID Study, United Kingdom (LINK)
A study of 427 pregnant women admitted to 194 UK hospitals suggests pregnant women are not at any higher risk from COVID-19 than non-pregnant women, and there is low risk of transmission from mother to baby in pregnancy or childbirth.
- Pregnant women are more at risk if they are of advanced age, have black/ethnic minority background, are overweight or obese, or have pre-existing medical conditions (e.g. diabetes and high blood pressure)
- The majority of pregnant women hospitalised for COVID-19 were in the third trimester of pregnancy
- 10% of the pregnant women in hospital required intensive care
- 2.5% of babies tested positive for the virus immediately after birth
- 5% of babies tested positive some time after birth
- 20% babies born to mothers hospitalised for COVID-19 were born prematurely and were admitted to a neonatal unit
Zhongnan Hospital of Wuhan University, Wuhan China (LINK)
A study of nine women with COVID-19 pneumonia in late pregnancy did not appear to show worse symptoms than non-pregnant persons. All babies were born from C-section and tested negative for the virus.
Samples of amniotic fluid, cord blood, newborn throat swabs and breast milk samples tested negative for COVID-19.
Qingdao Women and Children’s Hospital, China (LINK)
A study of one pregnant woman with COVID-19 showed similar symptoms to non-pregnant persons. The fetus showed signs of normal development throughout the study.
Union Hospital, Tongji Medical College, Huazhong University, Wuhan China (LINK)
A study of 15 pregnant women with COVID-19 pneumonia showed mild symptoms, with all achieving good recovery. All deliveries were successful, with no adverse infant outcomes.
Maternal and Child Health Hospital of Hubei Province, Union Hospital, Renmin Hospital, Tianmen First, People’s Hospital, Jingzhou Municipal Hospital and Child Health Hospital, and Pediatric Hospital affiliated with Fudan University, China (LINK)
A study of nine pregnant women with COVID-19 showed no cases of severe pneumonia or maternal death. There was one infant death. The 9 surviving newborns tested negative for COVID-19, but some experienced perinatal complications (i.e. complications immediately after birth). This included fetal distress (6 cases), premature birth (6 cases) and respiratory symptoms (7 cases).
The Second Affiliated Hospital and The Affiliated Infectious Hospital of Soochow University, Suzhou, China (LINK)
One pregnant woman with COVID-19 had a normal 30-week ultrasound but the baby shortly started showing decreased fetal movement and decreased heart rate. An emergency C-section delivered a preterm infant who consistently tested negative for COVID-19 for the study period. Placenta, amniotic fluid, umbilical cord blood, stomach juice and throat swab samples all tested negative.
Renmin Hospital of Wuhan University, Wuhan and the Central Hospital of Qianjiang City, Qianjiang, China (LINK)
16 pregnant women with COVID-19 were compared with 45 uninfected pregnant women. No significant differences were seen in pregnancy or birth outcomes (e.g. blood loss, birthweight, preterm birth, fetal distress). The 10 newborns who were tested were negative for COVID-19, although three were diagnosed with and successfully treated for bacterial pneumonia. Follow-up examinations after discharge from hospital showed all newborns were healthy.
Wuhan Children's Hospital, in Wuhan, Hubei Province, China (LINK)
33 babies born to women with COVID-19 were investigated for infection. Of the 33 babies, three were symptomatic for COVID-19. Consistent with other studies, clinical symptoms were mild and had favourable outcomes, with no reported deaths.

Connect with us